Brand Names: Various around the world
What is Gabapentin?
Gabapentin is a medicine that is used to treat a variety of disorders, including epilepsy, neuropathic pain, and restless leg syndrome. It is also an anticonvulsant and analgesic. As the text progresses, a comprehensive analysis of the uses and side effects of gabapentin will be presented. This generic medication is sold under a broad variety of brand names all over the world. A structural counterpart of the neurotransmitter gamma-aminobutyric acid (GABA), gabapentin was initially synthesised in 1977 by Parke-Davis, a Japanese pharmaceutical company. Gabapentin was initially used to treat Parkinson’s disease. In 1993, it was granted permission for usage in medical settings in the United States. In place of concentrating on brand names, this article will conduct an analysis of scientific journals and medical studies pertaining to the particular active ingredient gabapentin. Notable among these sources are the works of GC Quintero, BJ Mason et al., JG Leung et al., and ER Somerville et al., all of which offer excellent insights into the pharmacology, therapeutic uses, and potential hazards connected with the use of gabapentin.
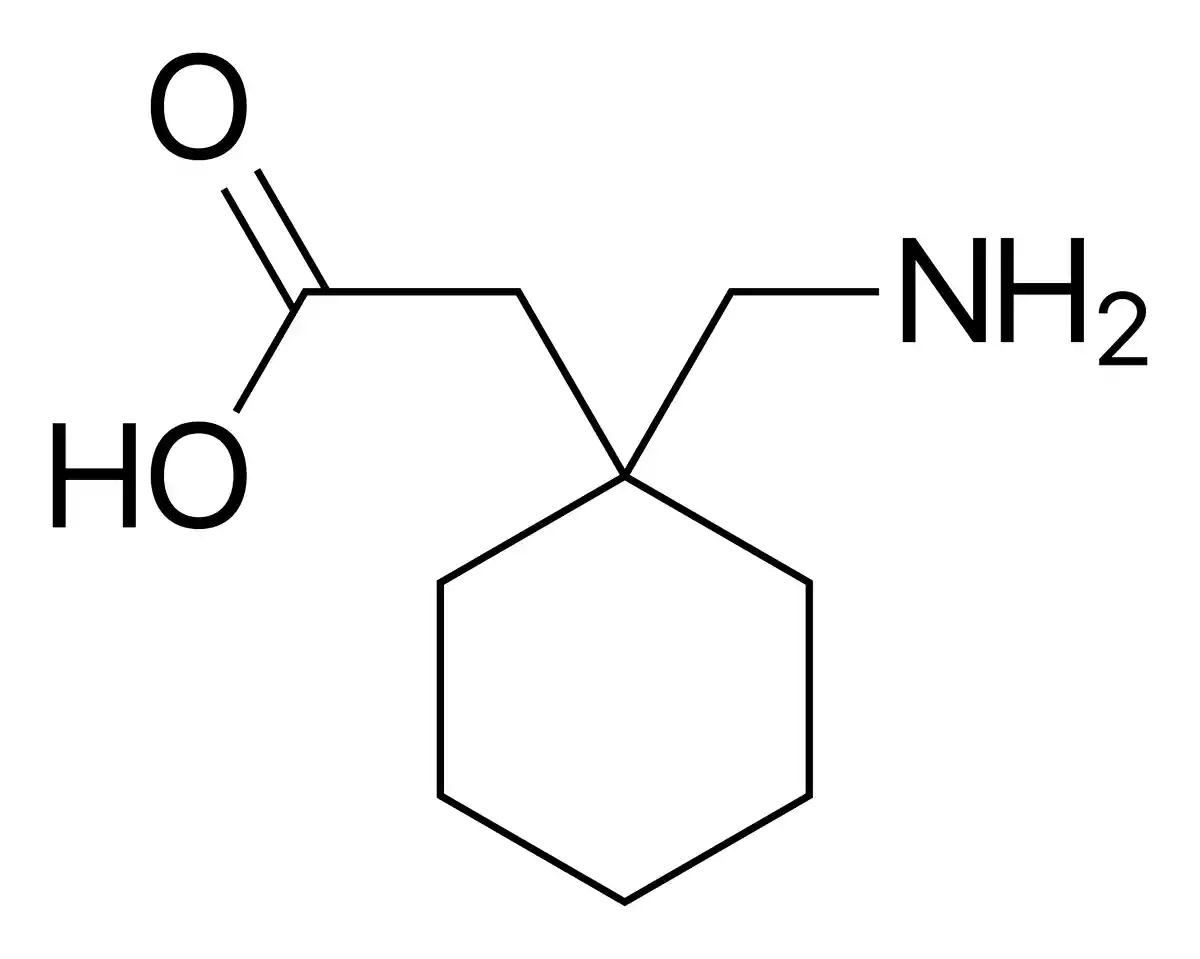
Chemical Structure and Mechanism of Action
Gabapentin, which is also known by its chemical name, 1-(aminomethyl)cyclohexaneacetic acid, is a structural analogue of the neurotransmitter GABA, which performs inhibitory functions. According to Quintero (2017), gabapentin does not bind directly to GABA receptors and does not appreciably change GABA absorption or breakdown. This is despite the fact that gabapentin is quite similar to GABA. The therapeutic benefits of this substance are thought to be exerted through a number of different pathways that are indirect. According to Somerville et al. (2015), one of the potential mechanisms includes the binding of gabapentin to the α2δ-1 subunit of voltage-gated calcium channels. This binding results in a decrease in calcium influx, which in turn leads to a decrease in neurotransmitter release at the same time. Attenuating neuronal excitability is one of the possible mechanisms that contributes to the anticonvulsant and analgesic actions of this substance. In addition, it has been demonstrated that gabapentin can modify the activity of specific enzymes, such as branched-chain amino acid aminotransferase, which may have an effect on the synthesis of neurotransmitters and the transmission of signals (Leung et al., 2015). Furthermore, according to Mason et al. (2018), gabapentin may have an influence on the dopaminergic and opioidergic systems, which could be the reason for its effectiveness in the management of alcohol withdrawal and dependence. On the other hand, the specific mechanisms that underlie the therapeutic activities of gabapentin continue to be the topic of continuing research and controversial dispute. The pharmacokinetic profile of the medication appears to be intricate and multi-dimensional, involving interactions with a variety of neurochemical systems and signalling pathways.
Indications
Gabapentin is prescribed for various medical conditions, including:
- Epilepsy: As an adjunctive therapy for partial seizures, with or without secondary generalisation, in adults and children aged 6 years and above (Somerville et al., 2015).
- Neuropathic pain: For the management of chronic neuropathic pain, such as postherpetic neuralgia, diabetic neuropathy, and trigeminal neuralgia (Quintero, 2017).
- Restless leg syndrome: To alleviate symptoms of restless leg syndrome, a neurological disorder characterised by an irresistible urge to move the legs (Leung et al., 2015).
- Alcohol withdrawal and dependence: Gabapentin has shown promise in managing alcohol withdrawal symptoms and promoting abstinence in individuals with alcohol use disorder (Mason et al., 2018).
Contraindications and Precautions
- Hypersensitivity: Gabapentin is contraindicated in patients with known hypersensitivity to the drug or its ingredients.
- Renal impairment: Dose adjustments are necessary for patients with renal insufficiency, as gabapentin is primarily eliminated via the kidneys.
- Pregnancy and lactation: Gabapentin should be used during pregnancy only if the potential benefits justify the risks. It is excreted in human milk; thus, caution is advised when administering to breastfeeding women.
- Suicidal ideation: Patients treated with gabapentin should be monitored for signs of suicidal thoughts or behaviour, as anticonvulsants have been associated with an increased risk of suicidal ideation.
Special Warnings for the Elderly, Children, and Pregnant Women
- Elderly: Gabapentin should be used with caution in elderly patients, as they may be more susceptible to adverse effects due to age-related changes in renal function and pharmacokinetics.
- Children: The safety and efficacy of gabapentin in children under 6 years of age have not been established. Close monitoring is required when prescribed to children.
- Pregnant women: Gabapentin should only be used during pregnancy if the potential benefits outweigh the risks. Pregnant women taking gabapentin should be enrolled in pregnancy registries to collect data on foetal outcomes.
Dosage and Administration
Gabapentin dosage varies depending on the indication and individual patient factors. The following are general dosing guidelines:
- Epilepsy: The initial dose is 300 mg three times a day, which can be titrated up to a maximum of 3,600 mg per day in divided doses.
- Neuropathic pain: The starting dose is typically 300 mg once daily, gradually increasing to 300 mg three times a day. The maximum dose is 3,600 mg per day in divided doses.
- Restless leg syndrome: The recommended dose ranges from 300 to 600 mg once daily, administered in the evening.
Dose adjustments may be necessary for patients with renal impairment or those on haemodialysis.
What Should I Do if I Miss a Dose?
If a dose of gabapentin is missed, it should be taken as soon as possible. However, if it is close to the time of the next scheduled dose, the missed dose should be skipped, and the regular dosing schedule should be resumed. Double doses should not be taken to compensate for a missed dose.
Uses
In addition to its approved indications, gabapentin has been studied for various off-label uses, such as:
- Anxiety disorders: Gabapentin may have anxiolytic properties and has been explored as a potential treatment for generalised anxiety disorder and social anxiety disorder (Quintero, 2017).
- Fibromyalgia: Some studies have suggested that gabapentin may help alleviate pain and improve sleep in patients with fibromyalgia (Leung et al., 2015).
- Hot flashes: Gabapentin has been investigated as a non-hormonal option for managing hot flashes in menopausal women and breast cancer survivors (Mason et al., 2018).
However, more research is needed to establish the efficacy and safety of gabapentin for these off-label applications.
Overdose
Gabapentin overdose can occur accidentally or intentionally. Symptoms of overdose may include:
- Drowsiness, lethargy, or sedation
- Ataxia or incoordination
- Slurred speech
- Dizziness or vertigo
- Nausea and vomiting
- Diarrhoea
- Double vision or other visual disturbances
- Tremors or muscle twitching
- Confusion or disorientation
- Respiratory depression (in severe cases)
Treatment for gabapentin overdose is primarily supportive and may involve gastric lavage, activated charcoal administration, or haemodialysis in severe cases (Leung et al., 2015).
Gabapentin Side Effects
Gabapentin side effects can range from mild to severe and may vary among individuals. It is essential for patients to be aware of potential adverse reactions and to report any concerning symptoms to their healthcare provider promptly.
Common Gabapentin Side Effects
- Drowsiness or somnolence
- Dizziness or lightheadedness
- Ataxia or unsteadiness
- Fatigue or weakness
- Nystagmus (involuntary eye movements)
- Tremor
- Peripheral oedema (swelling of the extremities)
- Nausea and vomiting
- Diarrhoea or constipation
- Dry mouth
- Weight gain
- Blurred vision
- Headache
These side effects are usually mild and may subside with continued use or dose adjustments (Quintero, 2017).
Rare but Possible Gabapentin Side Effects
- Mood changes, such as anxiety, depression, or agitation
- Confusion or disorientation
- Memory impairment
- Hallucinations or delusions
- Gynecomastia (breast enlargement in males)
- Rash or itching
- Alopecia (hair loss)
- Myalgia (muscle pain) or arthralgia (joint pain)
- Impotence or sexual dysfunction
- Pancreatitis
- Liver function abnormalities
- Blood dyscrasias, such as leucopenia or thrombocytopenia
These side effects are uncommon but may require medical attention if they persist or worsen (Mason et al., 2018).
Serious Gabapentin Side Effects
- Anaphylaxis or severe allergic reactions
- Angioedema (swelling of the face, tongue, or throat)
- Stevens-Johnson syndrome or toxic epidermal necrolysis (severe skin reactions)
- Suicidal thoughts or behaviour
- Respiratory depression
- Seizures (in non-epileptic patients)
- Withdrawal symptoms (if discontinued abruptly)
These side effects are rare but can be life-threatening. Patients experiencing any of these symptoms should seek immediate medical attention (Somerville et al., 2015).
Interactions
Gabapentin can interact with various drugs and substances, potentially altering its efficacy or increasing the risk of adverse effects.
Drug-Drug Interactions
- Antacids containing aluminium or magnesium: May reduce gabapentin absorption
- Opioids: May increase the risk of respiratory depression and sedation
- Alcohol: May enhance the sedative and cognitive effects of gabapentin
- Morphine: May increase gabapentin concentrations, leading to increased side effects
- Cimetidine: May decrease gabapentin clearance, resulting in higher blood levels
Patients should inform their healthcare provider about all medications they are taking to avoid potentially harmful interactions (Leung et al., 2015).
Drug-Food Interactions
There are no known significant drug-food interactions with gabapentin. However, it is generally recommended to take gabapentin with meals to minimise gastrointestinal side effects (Mason et al., 2018).
Additional Important Information
Resistance Development
In clinical practice, the development of resistance to gabapentin is not a big worry that people are concerned about. In contrast to antibiotics and antiviral drugs, which are designed to combat germs that are undergoing rapid mutations, gabapentin is a pharmaceutical that targets the neurological system of the human body. According to Somerville et al. (2015), the pharmacodynamic effects of gabapentin are mediated by its binding to the α2δ-1 subunit of voltage-gated calcium channels. This binding involves the modulation of neurotransmitter release and neuronal excitability. To the same extent as antimicrobial drugs are susceptible to the development of resistance, this method of action does not exhibit the same tendency. On the other hand, it is possible that individual patients will suffer a lessened therapeutic response over the course of treatment, which may require modifications to the dosage or the investigation of alternative possibilities for treatment. Rather than being a result of genuine pharmacological resistance to gabapentin, this phenomena is more likely to be linked to changes in the patient’s underlying illness or physiology.
Preclinical and Clinical Studies
In order to assess gabapentin’s effectiveness, safety, and possible uses, a great deal of research has been done on it in preclinical and clinical settings. Preclinical research has shed important light on the pharmacokinetic and pharmacodynamic characteristics of gabapentin, clarifying its modes of action and suggesting possible targets for treatment. For instance, the anticonvulsant and analgesic properties of gabapentin have been shown in animal models, opening the door for its clinical application in neuropathic pain and epilepsy (Quintero, 2017).
To evaluate gabapentin’s safety and effectiveness in a range of patient demographics and indications, clinical trials have been carried out. Since gabapentin has been shown to be effective in randomised controlled studies as an adjuvant treatment for partial seizures in both adults and children, this indication has been approved (Somerville et al., 2015). In a similar vein, clinical research has shown that gabapentin is useful in the treatment of neuropathic pain disorders such diabetic neuropathy and postherpetic neuralgia.
Apart from the approved indications, gabapentin has been explored for a number of off-label applications. Clinical trials have looked into the possibility of using gabapentin to treat fibromyalgia, alcohol use disorder, and anxiety disorders. In their evaluation of the data pertaining to the use of gabapentin for these reasons, Leung et al. (2015) emphasised the need for more studies to determine the drug’s safety and effectiveness in these situations.
One area of special study has been gabapentin’s effectiveness in treating alcohol abuse and withdrawal. Mason et al. (2018) have out an extensive analysis of the literature on this topic, looking at the available clinical evidence as well as probable mechanisms of action. The use of gabapentin in alcohol consumption disorder was found to have encouraging results; nevertheless, the authors also stressed the necessity for bigger, well-controlled trials to validate these results and direct clinical practice.
Preclinical and clinical research must continue as the therapeutic environment changes in order to clarify the possible uses and restrictions of gabapentin. Our knowledge of this adaptable drug will grow, enabling us to better employ it in therapeutic settings and enhance patient outcomes for a variety of neurological and psychiatric disorders.
Systematic Reviews and Meta-Analyses
Gathering the data on the effectiveness and safety of gabapentin for different applications has been made possible in large part by systematic reviews and meta-analyses. Informing clinical decision-making and the formulation of guidelines, these studies offer a thorough and objective evaluation of the literature. In a comprehensive review and meta-analysis, for instance, Wiffen et al. (2017) assessed how well gabapentin works for adult neuropathic pain. With a number required to treat (NNT) of 5.9 for a 50% decrease in pain, gabapentin was shown to be more pain-relieving than placebo in 37 trials with 5,914 subjects.
Peckham et al. (2018) conducted a further systematic review and meta-analysis to evaluate the safety and effectiveness of gabapentin in the treatment of alcoholism. With 1,128 individuals in all, the study comprised seven randomised controlled trials and concluded that, in comparison to placebo, gabapentin was significantly related with lower rates of excessive drinking and higher rates of abstention. Though further study is required to determine the best dosage schedules and to contrast gabapentin’s effectiveness with other pharmacological treatments, the authors came to the conclusion that it might be a viable therapy choice for alcohol consumption disorder.
Additionally pointing up possible gaps and doubts in the evidence base for gabapentin are systematic reviews and meta-analyses. In a systematic review and meta-analysis of gabapentin for fibromyalgia and neuropathic pain, for example, Moore et al. (2014) concluded that although gabapentin reduced pain, publication bias and poor study design and reporting limited the quality of the evidence. The authors underlined the need for high-quality, long-term trials to better guide clinical practice and evaluate the relative efficacy of gabapentin to other treatments.
Current Research Directions and Future Perspectives
Expanding the therapeutic uses of gabapentin, improving its clinical practice usage, and investigating new formulations and drug delivery technologies are the main goals of current study on the medicine. Preventing and treating postoperative pain with gabapentin is one interesting field of research. Perioperative gabapentin was shown to be useful as an adjuvant to multimodal analgesic regimes in a recent comprehensive review and meta-analysis by Fabritius et al. (2017). It also reduced postoperative pain ratings and opiate use.
The creation of gabapentin extended-release and controlled-release formulations, which seek to increase patient compliance and lower the incidence of side effects, is another vibrant field of study. The pharmacokinetic and pharmacodynamic characteristics of these new formulations were examined by Quintero (2017), who also pointed out some possible benefits over gabapentin released immediately. The author did point out, although, that further clinical research is required to determine their safety and effectiveness in relation to the conventional formulation.
Additionally being investigated is the use of gabapentin in the treatment of various neurological and mental illnesses including anxiety disorders, bipolar disorder, and sleep difficulties. Leung et al. (2015) looked at the body of research on the use of gabapentin for these conditions and found encouraging outcomes, especially for the treatment of sleeplessness and generalised anxiety disorder. Larger, well-controlled trials are still needed, the authors stressed, to support these results and direct clinical practice.
Future study can also concentrate on finding genetic or biomarker characteristics that forecast treatment response and side effects as our knowledge of gabapentin’s mechanisms of action develops. This could make gabapentin therapy more individualised by enabling doctors to customise treatment plans according to the unique features of each patient.
Finally, a mounting amount of data from systematic reviews, meta-analyses, and current research confirms that gabapentin is still a valuable treatment choice for a variety of neurological and psychiatric disorders. Additional research is required as the field of pharmacological treatments develops to maximise the use of gabapentin in clinical practice, investigate its potential in new indications, and create newer formulations that improve its effectiveness and tolerability. Working collaboratively, researchers and doctors can enhance patient outcomes and quality of life by deepening our knowledge of this adaptable drug.
In Brief
Gabapentin is an anticonvulsant and analgesic medication used to treat epilepsy, neuropathic pain, and restless leg syndrome. Neuronal excitability and neurotransmitter release are thought to be reduced as a result of its modulation of voltage-gated calcium channel function. Although most people handle gabapentin well, typical adverse effects include peripheral edoema, dizziness, and sleepiness. Reportedly rare yet dangerous side effects include respiratory depression and suicidal thoughts. Because gabapentin interacts with so many medications—including alcohol, opioids, and antacids—dosing must be carefully monitored. Although systemic reviews and meta-analyses have validated the usefulness of gabapentin for neuropathic pain and alcohol use disorder, more excellent research is still needed to determine the best dosage schedules and comparative effectiveness. The current research directions are to uncover biomarkers to predict therapy response, create new formulations, and broaden the therapeutic uses of gabapentin. Gabapentin is still a valuable treatment for many neurological and psychiatric disorders, and its usage in clinical practice should be optimised by continuous study as the body of evidence grows.
ATTENTION: It is crucial never to take medication without a qualified doctor’s supervision. Always read the Patient Information Leaflet (PIL) with each prescribed medicine. Pharmaceutical companies accurately describe each product’s details, which may be regularly updated, though variations may exist depending on the drug’s composition. This article analyses the active ingredient rather than specific brand names containing this generic medicine worldwide. Study the instruction leaflet for each preparation you use. Close cooperation with your doctor and pharmacist is vital. Self-administering medication carries serious health risks and must be strictly avoided.
Bibliography
- GC Quintero. (2017). Review about gabapentin misuse, interactions, contraindications and side effects. Journal of Experimental Pharmacology. tandfonline
- BJ Mason, S Quello, F Shadan. (2018). Gabapentin for the treatment of alcohol use disorder. Expert Opinion on Investigational Drugs. tandfonline
- JG Leung, D Hall-Flavin, S Nelson, et al. (2015). The role of gabapentin in the management of alcohol withdrawal and dependence. Annals of Pharmacotherapy. journals
- ER Somerville, AW Michell, A Sen. (2015). Gabapentin. The Treatment of Epilepsy. onlinelibrary


