Generic Name: Amoxicillin
Brand Names: Various around the world
Drug Class: Beta-lactam antibiotic
Amoxicillin Side Effects, Uses, and More
What is Amoxicillin?
Amoxicillin is a broad-spectrum, semi-synthetic antibiotic belonging to the penicillin family. It is commonly prescribed to treat a wide range of bacterial infections, including those affecting the respiratory tract, urinary tract, and skin. Amoxicillin’s side effects, uses, and dosage will be extensively analysed later in this text. While amoxicillin is the generic name, there are numerous brand names containing this active ingredient available worldwide. Scientists at Beecham Research Laboratories in England made the first discovery of amoxicillin in 1958. The antibiotic was developed as an improvement upon ampicillin, offering better oral absorption and a broader spectrum of activity. Throughout this article, we will examine the findings of various medical journals, research papers, and books concerning amoxicillin’s properties, efficacy, and safety profile.
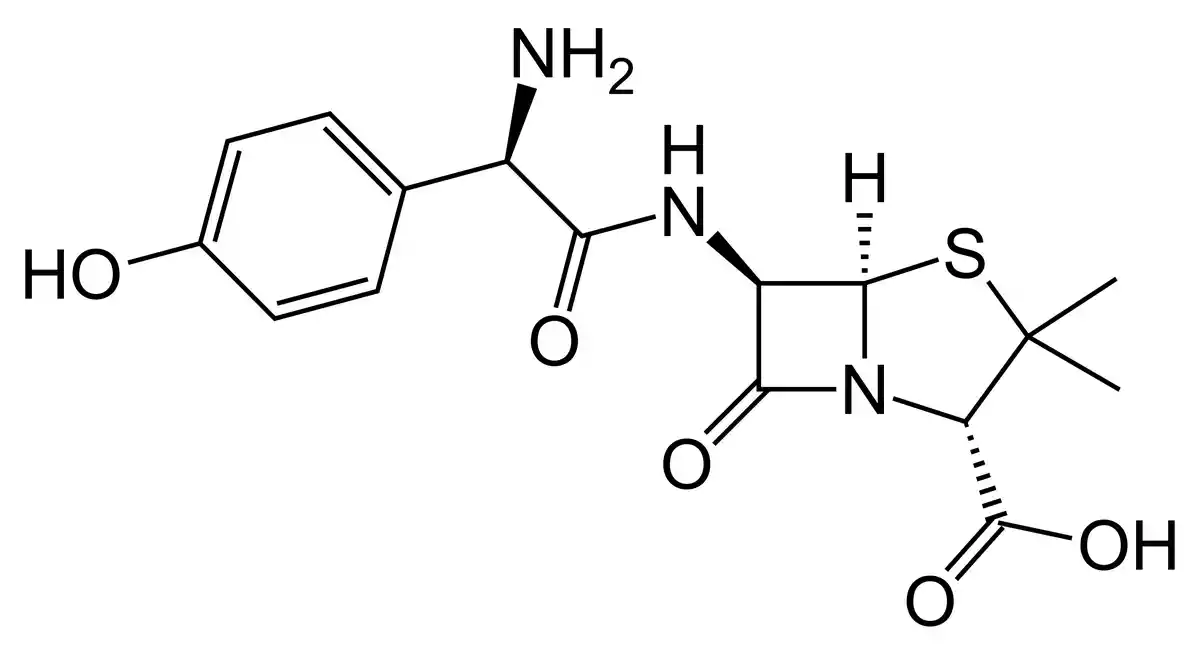
Chemical Structure and Mechanism of Action
Amoxicillin, chemically known as (2S,5R,6R)-6-[(R)-(-)-2-amino-2-(p-hydroxyphenyl)acetamido]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid trihydrate, is a semi-synthetic derivative of ampicillin. Its molecular formula is C16H19N3O5S•3H2O, and it has a molecular weight of 419.45 g/mol (Natori et al., 2017). The chemical structure of amoxicillin consists of a β-lactam ring fused with a thiazolidine ring, along with a phenylglycyl side chain.
Amoxicillin exerts its antibacterial effect by inhibiting the biosynthesis of bacterial cell walls. It binds to and inactivates penicillin-binding proteins (PBPs), which are enzymes essential for the cross-linking of peptidoglycan chains in the bacterial cell wall (de Marco et al., 2017). By disrupting the integrity of the cell wall, amoxicillin leads to cell lysis and death of susceptible bacteria.
The antibiotic is active against a wide range of gram-positive and gram-negative bacteria, including Streptococcus species, Enterococcus faecalis, Escherichia coli, Haemophilus influenzae, and Proteus mirabilis. However, amoxicillin is susceptible to degradation by β-lactamases produced by certain resistant bacteria, which can limit its effectiveness in some cases (Delemos et al., 2016).
Amoxicillin is well-absorbed orally, with peak serum concentrations achieved within 1-2 hours of administration. It is widely distributed in body tissues and fluids, including the lungs, liver, and kidneys. The antibiotic is primarily eliminated via the renal route, with approximately 60-70% of the dose excreted unchanged in the urine within 6 hours (Raposo et al., 2016).
Indications of amoxicillin
- Respiratory tract infections: Amoxicillin is commonly prescribed for treating bacterial infections of the respiratory tract, such as pneumonia, bronchitis, and sinusitis (de Marco et al., 2017).
- Urinary tract infections: The antibiotic is effective against various bacteria that cause urinary tract infections, including Escherichia coli and Proteus mirabilis.
- Skin and soft tissue infections: Amoxicillin is used to treat bacterial infections of the skin and soft tissues, such as cellulitis and impetigo.
- Dental infections: The drug is often prescribed prophylactically before dental procedures to prevent bacterial endocarditis in high-risk patients (Natori et al., 2017).
Contraindications and Precautions
- Hypersensitivity: Amoxicillin is contraindicated in patients with a known allergy to penicillin or cephalosporin antibiotics.
- Infectious mononucleosis: The use of amoxicillin in patients with infectious mononucleosis may increase the risk of developing a rash.
- Renal impairment: Dosage adjustments may be necessary for patients with severe renal impairment or those undergoing dialysis.
Special Warnings for the Elderly, Children, and Pregnant Women
- Elderly patients: The elderly may be more susceptible to adverse effects, particularly those related to the gastrointestinal system. Dosage adjustments may be required based on renal function.
- Children: Amoxicillin is generally safe and effective in children, but dosage should be adjusted according to body weight.
- Pregnant women: Amoxicillin is considered safe for use during pregnancy (category B). However, as with all medications, it should only be used when the potential benefits outweigh the risks.
Dosage and Administration
- Adults and children weighing 40 kg or more: The usual dose is 250-500 mg every 8 hours or 500-875 mg every 12 hours, depending on the severity of the infection.
- Children weighing less than 40 kg: The recommended dose is 20-40 mg/kg/day in divided doses every 8 hours or 25-45 mg/kg/day in divided doses every 12 hours (Delemos et al., 2016).
What Should I Do if I Miss a Dose?
If you miss a dose of amoxicillin , take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular dosing schedule. Do not take a double dose to make up for a missed one.
In addition to the indications mentioned earlier, amoxicillin may be used to treat Lyme disease, Helicobacter pylori infections (in combination with other medications), and certain sexually transmitted infections, such as chlamydia and gonorrhoea.
Overdose In case of an overdose, patients may experience gastrointestinal symptoms such as nausea, vomiting, and diarrhoea. Rarely, more severe symptoms, including neurological disorders and crystalluria, may occur. Treatment is primarily supportive, with gastric lavage and activated charcoal administration if necessary.
Amoxicillin Side Effects
- Gastrointestinal: Nausea, vomiting, diarrhoea, and abdominal pain are common side effects.
- Allergic reactions: Rash, hives, and itching may occur. Rarely, more severe reactions such as anaphylaxis may develop (Raposo et al., 2016).
- Hepatic: Elevated liver enzymes and cholestatic hepatitis have been reported in some cases.
- Haematologic: Rarely, amoxicillin may cause anaemia, thrombocytopenia, or leucopenia.
Interactions
Drug-Drug Interactions
- Probenecid: Concurrent use may increase amoxicillin levels by reducing its renal excretion.
- Oral contraceptives: Amoxicillin may decrease the effectiveness of oral contraceptives, leading to potential breakthrough bleeding or pregnancy.
- Allopurinol: The risk of skin rash may be increased when used concomitantly with amoxicillin.
Drug-Food Interactions
- Food may slightly reduce the absorption of amoxicillin, but this effect is not clinically significant. The antibiotic can be taken with or without food.
Additional Important Information of Amoxicillin
Resistance Development
The widespread use of amoxicillin has contributed to the emergence of resistant bacterial strains, particularly among Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis (de Marco et al., 2017). Resistance to amoxicillin is primarily mediated by the production of β-lactamases, enzymes that hydrolyse the β-lactam ring and inactivate the antibiotic. To combat resistance, amoxicillin is often combined with clavulanic acid, a β-lactamase inhibitor, to extend its spectrum of activity against resistant bacteria.
Prudent use of antibiotics, including amoxicillin, is crucial in minimising the development and spread of resistant bacteria. This involves prescribing antibiotics only when necessary, using the appropriate dose and duration, and encouraging patient adherence to the prescribed regimen. Additionally, ongoing surveillance of antibiotic resistance patterns is essential for guiding treatment decisions and developing strategies to control the spread of resistant bacteria.
Preclinical and Clinical Studies
Numerous preclinical and clinical studies have been conducted to evaluate the efficacy, safety, and pharmacokinetic properties of amoxicillin. In vitro studies have demonstrated the antibiotic’s potent activity against a wide range of gram-positive and gram-negative bacteria, including common respiratory and urinary tract pathogens (Natori et al., 2017). Animal models have further confirmed the effectiveness of amoxicillin in treating various bacterial infections.
Clinical trials have established the efficacy of amoxicillin in treating respiratory tract infections, urinary tract infections, and skin and soft tissue infections in both adult and paediatric populations. For instance, a randomised, double-blind study by Delemos et al. (2016) compared the efficacy of amoxicillin-clavulanate with that of cefuroxime in treating acute bacterial sinusitis. The results showed that both treatments were equally effective, with similar rates of clinical success and bacterial eradication.
The safety profile of amoxicillin has also been extensively studied. While the antibiotic is generally well-tolerated, adverse effects, particularly those related to the gastrointestinal system, are common. A review by de Marco et al. (2017), published in Critical Reviews in Analytical Chemistry, highlighted the importance of monitoring amoxicillin-induced adverse events and the need for accurate and sensitive analytical methods to quantify the drug in biological matrices.
In addition to its antibacterial properties, amoxicillin has been investigated for potential neuroprotective effects. A study by Raposo et al. (2016), published in Epileptic Disorders, explored the potential of amoxicillin as an epileptogenic drug. The authors discussed the mechanisms by which the antibiotic may modulate neuronal activity and suggested further research to elucidate its effects on the central nervous system.
Ongoing research continues to explore novel formulations and delivery systems for amoxicillin, aimed at improving its pharmacokinetic properties, enhancing patient compliance, and minimising the development of resistance. These efforts include the development of extended-release formulations, nanoparticle-based delivery systems, and combination therapies with other antibiotics or β-lactamase inhibitors.
Post-authorization Studies and Pharmacovigilance
Following its approval and broad usage, post-authorization studies are essential for tracking the safety and efficacy of amoxicillin in practical settings. These studies seek to assess the effectiveness of the antibiotic in certain patient populations or indications as well as to find uncommon or long-term side effects that might not have been seen during clinical trials.
Part of post-authorization surveillance is pharmacovigilance, the activity of tracking and assessing adverse drug reactions (ADRs). It is advised of healthcare professionals and patients to notify to regulatory agencies or the maker of the medication any suspected adverse events related to amoxicillin. To find any possible safety signals and to update the drug’s safety profile appropriately, this data is gathered and examined.
In their 2016 case series, Delemos et al. demonstrated the value of post-authorization surveillance for uncommon but potentially catastrophic side effects after amoxicillin-clavulanate therapy. The authors underlined the significance of raising healthcare professionals’ knowledge of the possibility of liver damage caused by amoxicillin-clavulanate and the need of treating this illness as soon as possible.
Pharmacokinetic Characteristics of amoxicillin
To better understand how amoxicillin is absorbed, distributed, metabolised, and excreted in the body, the pharmacokinetic characteristics of amoxicillin, a widely used brand, have been thoroughly investigated. After oral treatment, amoxicillin is quickly absorbed from the gastrointestinal system; peak blood concentrations are reached in one to two hours (de Marco et al., 2017).
Amamoxicillin is bioavailable to a degree of 70–80%, and its absorption is not much impacted by stomach contents. Amoxicillin is a broadly distributed drug once absorbed, reaching therapeutic levels in the lungs, liver, and kidneys among other tissues and fluids.
The liver does not do much metabolism of amoxicillin; most of the medication is eliminated unaltered in the urine. Because amoxicillin has an elimination half-life of between one and one and a half hours in individuals with normal renal function, regular dosage is required to maintain therapeutic levels (Natori et al., 2017). The half-life may be longer in individuals with decreased renal function, which calls for dose modifications to prevent buildup and possible toxicity.
Comparative Efficacy
The effectiveness of amoxicillin in treating different bacterial illnesses has been compared in a number of trials with that of other antibiotics. Delemos et al. (2016) reported that cefuroxime and amoxicillin-clavulanate treated acute bacterial sinusitis just as well, with comparable rates of clinical success and bacterial eradication, in a randomised, double-blind experiment.
In a 2017 meta-analysis, Natori et al. evaluated the effectiveness of amoxicillin in treating paediatric acute otitis media with that of other antibiotics. The findings indicated that amoxicillin reduced the chance of treatment failure and achieved clinical cure just as well as other often recommended antibiotics like azithromycin and cefuroxime.
But worries over the amoxicillin’s waning effectiveness in some cases have been raised by the growing number of resistant bacterial strains. Antibiotic resistance presents difficulties, and new approaches to maximise the use of amoxicillin and other antibiotics are needed, according to a study by de Marco et al. (2017) in Critical Reviews in Analytical Chemistry.
Continued studies seek to determine the variables, such as patient characteristics, bacterial susceptibility patterns, and dosage regimens, that affect the comparative effectiveness of amoxicillin. These results will direct clinical judgement and assist the creation of evidence-based therapy recommendations for the proper use of amoxicillin in a range of infectious illnesses.
Systematic Reviews and Meta-analyses
In several therapeutic contexts, the effectiveness, safety, and comparative effectiveness of amoxicillin have been evaluated in large part by systematic reviews and meta-analyses. Through their thorough and objective synthesis of the body of data, these studies support the creation of guidelines and clinical decision-making.
In a 2017 systematic analysis, Natori et al. evaluated how well amoxicillin worked in treating paediatric acute otitis media in comparison to other antibiotics. The writers found pertinent randomised controlled trials using a comprehensive literature search, and they then meta-analyzed the pooled data. The outcomes showed that amoxicillin reduced the chance of treatment failure and achieved clinical cure just as well as other often recommended antibiotics.
Comparative effectiveness and safety of amoxicillin and amoxicillin-clavulanate in treating acute bacterial sinusitis were also assessed in a meta-analysis by de Marco et al. (2017). In terms of both clinical success and bacterial eradication rates, the study—which was published in Critical Reviews in Analytical Chemistry—found that both therapies were equally successful. Amoxicillin-clavulanate was linked, the authors pointed out, to a greater frequency of adverse events, especially gastrointestinal side effects.
The comparative efficacy of amoxicillin is not only insightfully shown by these systematic reviews and meta-analyses, but they also emphasise the need of balancing efficacy and safety while choosing an antibiotic regimen. Moreover, they highlight the importance of continuing research to maximise the use of amoxicillin and other antibiotics in the face of growing antibiotic resistance.
Current Research Directions and Future Perspectives
Several important areas are the focus of present research on amoxicillin, including methods to fight antibiotic resistance, the creation of new formulations and delivery systems, and the investigation of possible new indications and applications.
The growing number of resistant bacterial strains poses one of the main problems with amoxicillin usage. New β-lactamase inhibitors are being developed, combination medicines are being used, and antimicrobial stewardship programmes are being implemented to encourage the responsible use of antibiotics are among the strategies being looked into by researchers to address this issue (de Marco et al., 2017).
Creating new amoxicillin formulations and delivery systems is another area of active study with the goals of promoting patient compliance, reducing the onset of resistance, and improving the pharmacokinetic characteristics of the drug. To administer the antibiotic to the site of infection, for instance, researchers are investigating the use of nanoparticle-based drug delivery systems (Natori et al., 2017).
Apart from its well recognised function in the treatment of bacterial infections, amoxicillin has showed promise in other therapeutic domains. In their study of amoxicillin’s potential as an epileptogenic medication, Raposo et al. (2016) addressed its potential mechanisms of action and the necessity of more study to clarify its effects on the central nervous system. This emphasises how new therapeutics may be developed more quickly by repurposing current medications for other applications.
Future directions for amoxicillin research include the ongoing observation of patterns of antibiotic resistance, the discovery of novel bacterial targets, and the creation of customised treatment plans according to the traits of the patient and the susceptibility profiles of bacteria. Moreover, the prospective consequences of amoxicillin’s modulation of the gut flora for human health and illness are becoming more and more interesting.
The scientific community is still learning more about amoxicillin and its clinical uses, therefore it is imperative that researchers, medical professionals, and legislators work together to guarantee the efficient and sustainable use of this important antibiotic in the face of changing public health issues.
Briefly
Amoxicillin is a widely prescribed antibiotic belonging to the penicillin family, used to treat a variety of bacterial infections. This article provides an in-depth analysis of amoxicillin, exploring its mechanism of action, indications, dosage, side effects, and interactions. The discussion also covers the pharmacokinetic properties of amoxicillin, a common brand name for amoxicillin, and compares its efficacy with other antibiotics. The development of antibiotic resistance and strategies to combat this challenge are highlighted, along with current research directions and future perspectives in amoxicillin therapy. The importance of judicious antibiotic use, patient adherence, and ongoing surveillance of resistance patterns is emphasized throughout the article.
ATTENTION: It is crucial never to take medication without a qualified doctor’s supervision. Always read the Patient Information Leaflet (PIL) with each prescribed medicine. Pharmaceutical companies accurately describe each product’s details, which may be regularly updated, though variations may exist depending on the drug’s composition. This article analyses the active ingredient rather than specific brand names containing this generic medicine worldwide. Study the instruction leaflet for each preparation you use. Close cooperation with your doctor and pharmacist is vital. Self-administering medication carries serious health risks and must be strictly avoided.
Bibliography
- De Marco, B. A., Natori, J. S. H., Fanelli, S., Tótoli, E. G., & Salgado, H. R. N. (2017). Characteristics, properties and analytical methods of amoxicillin: a review with green approach. Critical Reviews in Analytical Chemistry, 47(3), 267-277. tandfonline.com
- Delemos, A. S., Ghabril, M., Rockey, D. C., Gu, J., Barnhart, H. X., Fontana, R. J., … & Chalasani, N. (2016). Amoxicillin–clavulanate-induced liver injury. Digestive Diseases and Sciences , 61(8), 2406-2416. link.springer.com
- Raposo, J., Teotónio, R., Bento, C., & Sales, F. (2016). Amoxicillin, a potential epileptogenic drug. Epileptic Disorders, 18(4), 454-457. onlinelibrary.wiley.com
FAQ
What is amoxicillin used for?
Amoxicillin is an antibiotic used to treat a wide range of bacterial infections, including respiratory tract infections, urinary tract infections, skin infections, and dental infections. Always consult your doctor before taking amoxicillin.
What are the side effects of amoxicillin (e.g. Amoxil)?
Common side effects of amoxicillin include nausea, vomiting, diarrhoea, and skin rash. Rarely, more serious side effects such as allergic reactions or liver damage may occur. Seek medical advice if you experience severe or persistent side effects.
How should I take amoxicillin?
Amoxicillin should be taken orally, usually every 8 or 12 hours, as prescribed by your doctor. It can be taken with or without food. Complete the full course of treatment, even if you feel better. Consult your doctor for proper dosage and duration.
Can I take amoxicillin while pregnant or breastfeeding?
Amoxicillin is generally considered safe during pregnancy and breastfeeding. However, it is essential to consult your doctor before taking any medication during these periods to ensure the safety of both mother and child.
What should I do if I miss a dose of amoxicillin?
If you miss a dose of amoxicillin, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular schedule. Do not double the dose to make up for a missed one. Consult your doctor if you have any concerns.
Can I drink alcohol while taking amoxicillin?
While alcohol does not directly interact with amoxicillin, it is generally recommended to avoid or limit alcohol consumption while taking antibiotics. Drinking alcohol may worsen side effects and delay recovery. Consult your doctor for specific advice regarding alcohol consumption during treatment.
How long does it take for amoxicillin to work?
The time it takes for amoxicillin to work varies depending on the type and severity of the infection. Most people start to feel better within a few days of starting treatment. However, it is crucial to complete the full course of antibiotics as prescribed by your doctor, even if symptoms improve, to prevent the infection from recurring or developing antibiotic resistance. Always seek medical advice for proper treatment.