Generic Name: Codeine
Brand Names: Various around the world
Drug Class: Opioid analgesic
Codeine Side Effects: Uses, Dosage, and More
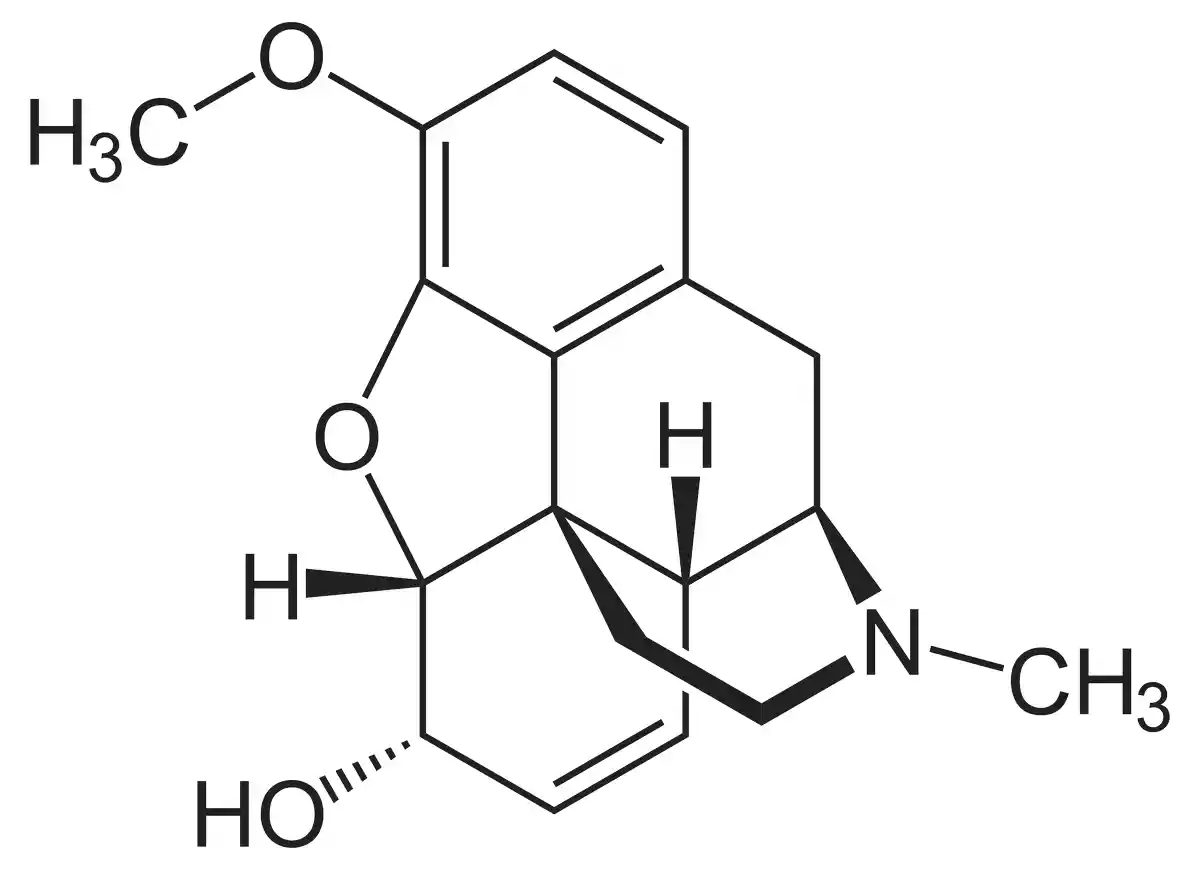
What is Codeine? – Chemical Structure and Mechanism of Action
Codeine is an opioid medication used to treat mild to moderately severe pain and suppress coughing. It falls under the family of opioids known as analgesics. From the opium poppy plant, codeine is chemically an alkaloid produced. Its structure comprises a methylation nitrogen bridge around a phenanthrene nucleus.
Codeine exerts its effects by binding to mu-opioid receptors in the central nervous system. A part of codeine is metabolised once consumed to morphine, which is mostly responsible for its analgesic effects. Additionally directly on medulla cough receptors, codeine suppresses the cough reflex.
Codeine is an opioid so it has negative effects and dependency problems. Prescription versions of it are available in several nations; others let low-dose codeine formulations be sold over-the-counter. Many pharmaceutical firms across the globe sell codeine-containing medications under different brand names. When conventional therapies are insufficient, codeine is recommended for temporary control of acute discomfort and coughing suppression.
History of Medicine
Codeine was first isolated from opium in 1832 by French chemist Pierre Robiquet. It became widely used as a pain reliever and cough suppressant in the late 19th century. Codeine’s discovery marked an important advancement in the development of opioid medications.
Recent research has examined codeine’s pharmacology, efficacy, and safety profile. Studies have investigated topics such as genetic variations affecting codeine metabolism, potential for misuse, and comparative effectiveness versus other analgesics. This article will analyze several key studies on codeine published in medical journals.
Uses of Codeine
Mostly acting as an analgesic for mild to moderate pain and as an antitussive to stop coughing, codeine Its analgesic properties help to control acute pain from dental work, surgery, traumas, or several medical disorders. Codeine acts as a cough suppressant, therefore helping to reduce non-productive, recurring coughing linked with different respiratory conditions.
Low-dose codeine concoctions are sold over-the-counter in certain areas, usually mixed with other analgesics such as paracetamol. Stronger formulas, however, call for a prescription. When non-opioid treatments are insufficient, doctors may write codesine prescriptions for temporary pain relief.
Codeine’s effectiveness in comparison to other painkillers has lately attracted attention in studies Variations in codeine use across European nations were revealed by a study by Hockenhull et al. titled “The association between the availability of over the counter codeine and the prevalence of non-medical use”. This underlines the need of careful regulation (European Journal of Clinical Pharmacology).
Contraindications and Precautions
Patients with known hypersensitivity to opioids, severe respiratory depression, acute asthma episodes, or paralytic ileus should not take codeine. For those with head traumas, elevated intracranial pressure, or compromised breathing ability, caution is advised.
Users of codeine run more danger for patients with a history of drug misuse or addiction. Particularly for long-term usage, the medication’s potential for dependency calls for great thought before being prescribed.
Interactions between other central nervous system depressants—alcohol, benzodiazepines, and other opioids—can intensify sedation and respiratory depression. Before beginning codeine treatment, doctors should carefully go over a patient’s drug history.
Special Warnings for the Elderly, Children, and Pregnant Women
Older individuals may have more susceptibility to the effects of codeine, which would call for dosage changes and constant observation. Common in older persons, impaired renal or hepatic function might impact codeine metabolism and clearance.
Children’s usage of codeine has drawn criticism because of safety issues. After reports of severe respiratory depression in ultra-rapid metabolizers, several nations have limited or outlawed its usage in young populations. When contemplating codeine for children, careful evaluation of risks and benefits is very essential.
Only if the possible benefit exceeds the danger to the baby should pregnant women consume codeine. Pregnancy-related prolonged usage could cause newborn opioid withdrawal syndrome. Breastfeeding women should be careful as codeine and its metabolites may enter into breast milk and could harm the baby.
Dosage and Administration
Dosing codeine depends on the indication, formulation, and personal patient characteristics. Typical oral dosages for people seeking pain treatment range from 15 to 60 mg every 4 to 6 hours as required, not more than 360 mg daily. Usually requiring smaller doses—often 10 to 20 mg every 4 to 6 hours—cough control calls for less.
Particularly in patients who are opioid-naive, healthcare professionals should start therapy at the lowest effective dosage and titrate cautiously. Minimizing the danger of dependency requires constant evaluation of the need for ongoing codeine treatment.
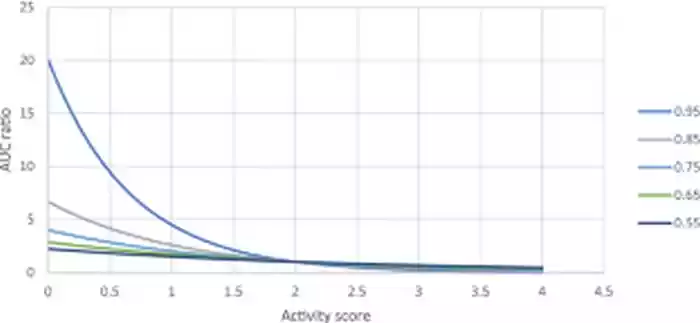
Personalized dosage based on genetic variables influencing codeine metabolism is highlighted in a paper by Saab and Nakad, “A software tool to adjust codeine dose based on CYP2D6 gene-pair polymorphisms and drug-drug interactions,” The Pharmacogenomics Journal reports.
What Should I Do If I Miss a Dose?
Patients should take a missed dosage as soon as they recall, unless it falls around the time for the next planned dosage. Under such circumstances, it is suggested to omit the missed dosage and start the usual dosing pattern once more. Doubling up on dosages to make up for a missed one should be avoided as it might cause side effects.
If unclear about how to continue after missing a dosage, patients should see their pharmacist or healthcare practitioner particularly if they use codeine for chronic pain management or as part of a planned treatment course.
Overdose
Mostly from respiratory depression, a codeine overdose may be fatal. Among the symptoms include great tiredness, bewilderment, cold and clammy skin, pinpoint pupils, slow or shallow breathing, and loss of consciousness. Severe forms might cause death or coma. In suspected overdose events, quick medical intervention is very vital.
Usually include supportive care, treatment may also include naloxone, an opioid antagonist with fast reversal of respiratory depression. Should the overdose be recent and the patient remain aware, activated charcoal might be utilized.
Higher dosages, concomitant use of other central nervous system depressants, or in those with impaired opioid metabolism increase the risk of overdose. To reduce overdose risk, Zarin et al. underline the need of knowing the pharmacology of codeine (Pharmaceutics).
Interactions
Drug-drug interactions
Many drugs interact with codeine, therefore either its effectiveness or risk of side effects may change. Other opioids, benzodiazepines, monoamine oxidase inhibitors (MAOIs), CYP2D6 inhibitors, and CYP3A4 inducers or inhibitors abound in notable combinations.
Combining codeine with other opioid analgesics causes cumulative central nervous system depression. Concurrent usage with benzodiazepines could boost sedative effects and raise respiratory depression risk. Strong enhancement of codeine’s effects by MAOIs may cause serotonin syndrome.
Medications that block CYP2D6—such as several antidepressants—can lessen codeine’s analgesic action by stopping its conversion to morphine. Codeine metabolism may be changed by CYP3A4 inducers or inhibitors, therefore influencing its safety and effectiveness profile.
The study by Saab and Nakad underlines the need of taking genetic differences in CYP2D6 into account when evaluating possible medication interactions (The Pharmacogenomics Journal).
Drug-food interactions
Although less frequent than drug-drug interactions, several meals and drinks may influence the way codeine is metabolised and thus its efficacy. Grapefruit juice may block CYP3A4, therefore raising the body’s codeine levels. Alcohol raises the likelihood of respiratory depression and aggravates central nervous system depression. For immediate-release formulations, high-fat meals might cause delay in starting of action.
Patients should discuss possible food interactions and dietary restrictions as well as codeine use with healthcare practitioners.
Codeine Side Effects
Typical side effects include dry mouth, constipation, nausea and vomiting, sleepiness and dizziness, and itching. Usually, these adverse effects pass when the body becomes used to the medicine. But persistent or severe symptoms call for professional help.
Variations in the frequency of codeine-related adverse effects observed by Hockenhull et al. amongst several European nations underlined the necessity of uniform monitoring and reporting methods (European Journal of Clinical Pharmacology).
Rare but Possible Codeine Side Effects
Though less frequent, some people might have more severe side effects. These may include severe respiratory depression, allergic responses (including anaphylaxis), serotonin syndrome (when paired with certain drugs), adrenal insufficiency with long-term usage, and raised intracranial pressure.
In their investigation on codeine phosphate solubility, Sodeifian et al. subtly highlight the need of correct formulation in reducing side effects (Scientific Reports).
How to Manage Codeine Side Effects
Good control of side effects helps to enhance patient outcomes and treatment adherence. Increasing hydration and fiber consumption as advised by a healthcare expert as well as contemplating stool softeners or laxatives may assist with constipation. Unless directed otherwise, taking codeine with meals may help reduce nausea. Should nausea continue, antiemetic drugs might be recommended.
Patients should not drive or operate equipment until the impact on alertness is understood if they are prone to sleepiness. Maybe dosage changes are required. For itching, antihistamines may help. See a healthcare provider if severe or ongoing. Staying hydrated and utilizing sugar-free gum or lozenges to boost salivation production may help with dry mouth.
More severe side effects need for quick medical intervention. Patients should be informed about possible side effects and when to visit an emergency room. Regular visits to healthcare professionals let one continuously evaluate the benefit-risk ratio of codeine treatment. If adverse effects continue or greatly affect quality of life, dose changes or other painkillers might be taken under consideration.
According to Zarin et al., continuous study on codeine analogues could provide better side effect profiles in next painkillers (Pharmaceutics). This emphasizes how dynamically changing opioid pharmacology is and the possibility for more focused treatments with less side effects.
Additional Important Information of Codeine
Genetic variations in metabolizing enzymes provide great variation in the pharmacokinetic profile of codeine. The drug mostly converts to morphine by means of significant first-pass metabolism under CYP2D6. Its analgesic effects depend on this conversion as codeine itself has quite modest opioid receptor affinity. Interindividual variations in CYP2D6 activity may cause significant changes in profiles of side effects and analgesic response.
Efforts at pharmacovigilance have been more intense recently, with an emphasis on the hazards related to codeine use—especially in young populations. Studies of post-authorization data have raised questions about respiratory depression in ultra-rapid codeine metabolizers of youngsters. These results have led governments all over to review and limit codeine usage in certain patient categories.
The pharmacodynamics and possible pharmacological interactions of codeine are still under investigation in preclinical investigations. Underlining the shift towards personalized medicine in pain treatment, research by Saab and Nakad has produced a software tool for customizing codeine dose based on CYP2D6 gene-pair polymorphisms and drug-drug interactions (The Pharmacogenomics Journal).
Extended usage of codeine may cause resistance development to its analgesic properties, which calls for either other pain management techniques or dosage increase. Tolerance mechanisms and opioid receptor desensitization help to explain this phenomena. Still, especially with long-term or high-dose use, the potential of physical dependency and addiction remains a major issue.
Clinical research on the safety and effectiveness of codeine across many indications have looked at great detail. Recent studies have focused on maximizing dose schedules, looking at combo treatments, and evaluating how genetic variables affect therapy results. The continuous study seeks to strike a compromise between analgesic effectiveness and minimum side effects and misuse potential.
Effectiveness
In codeine pharmacology, current research interests span numerous important domains. Development of new formulations and delivery technologies to improve bioavailability and lower negative effects is one area of concentration. Zarin et al. address the synthesis and modification of codeine derivatives, stressing possible directions for developing better pain relieving drugs with more acceptable pharmacological characteristics (Pharmaceutics).
Studies of relative effectiveness have compared codeine with various analgesics and antitussives. These studies seek to determine the ideal position of codeine in systems of pain management and cough control. Results have been conflicting; some studies show equivalent effectiveness to non-opioid substitutes for various reasons, while others show better pain relief in particular patient groups.
Meta-analyses and systematic reviews have given insightful analysis of codeine’s general safety and efficacy. These thorough analyses combine information from many clinical studies to provide a more all-encompassing view of the therapeutic worth of the medication. Recent meta-analyses have focused on codeine’s roles in pediatric cough suppression, chronic non-cancer pain, and postoperative pain management.
One prominent topic of research is how availability of codeine influences non-medical usage habits. Hockenhull et al. looked examined the correlation between non-medical usage frequency across many European nations and over-the-counter codeine availability. Their results underscore the importance of balanced approaches to codeine availability because they imply a complicated interaction between regulatory measures and usage patterns (European Journal of Clinical Pharmacology).
Future directions in codeine research include investigating new medication combinations to improve effectiveness while lowering risk. Furthermore, there is increasing interest in creating alternative opioid analgesics with better safety profiles, maybe using knowledge from the pharmacological features of codeine.
Reevaluation of codeine’s position in treatment regimens has been motivated by changing pain management terrain and growing worries about opioid abuse. Constant research seeks to improve patient selection criteria, maximize dose policies, and provide more focused methods of pain treatment. These initiatives acknowledge the requirement of cautious risk-benefit analysis in the use of codeine and indicate the ongoing relevance of it in clinical practice.
Analysis of the Research Study “A software tool to adjust codeine dose based on CYP2D6 gene-pair polymorphisms and drug-drug interactions”
This study, conducted by Yolande Saab and Zahi Nakad and published in The Pharmacogenomics Journal in 2023, presents an innovative approach to personalized medicine in the context of codeine administration. The research addresses the critical issue of variability in codeine metabolism due to genetic factors and drug interactions.
Methodology and Key Findings
The authors developed a software tool designed to optimize codeine dosing by considering two crucial factors:
- CYP2D6 gene-pair polymorphisms: These genetic variations significantly affect how individuals metabolize codeine into its active form, morphine.
- Drug-drug interactions: The tool accounts for potential interactions between codeine and other medications that might alter its metabolism or efficacy.
Significance of the Research
Personalized Medicine Approach
This study represents a significant step towards personalized pain management. By tailoring codeine doses based on individual genetic profiles and concurrent medications, the tool aims to:
- Enhance therapeutic efficacy
- Reduce the risk of adverse effects
- Minimize the potential for overdose or underdose
Clinical Implications
The software tool has the potential to revolutionize codeine prescription practices. It could enable healthcare providers to:
- Make more informed decisions about codeine dosing
- Predict patient response to codeine more accurately
- Adjust treatment plans proactively based on genetic and pharmacological factors
Limitations and Future Directions
While the study presents a promising approach, several limitations and areas for future research emerge:
- Validation in Clinical Settings: The tool’s effectiveness needs to be validated in diverse patient populations and real-world clinical scenarios.
- Integration with Electronic Health Records: Future research should explore how this tool can be seamlessly integrated into existing healthcare systems.
- Expanding to Other Opioids: The principles applied in this study could potentially be extended to other opioid medications with variable metabolism.
Critical Analysis
The study by Saab and Nakad addresses a crucial gap in pain management practices. The variability in codeine metabolism has long been a challenge in clinical settings, often leading to suboptimal pain control or increased risk of side effects. By leveraging genetic information and considering drug interactions, this software tool represents a significant advancement in the field of pharmacogenomics.
However, the practical implementation of such a tool faces several challenges:
- Accessibility of Genetic Testing: Widespread use of the tool would require readily available and affordable genetic testing for CYP2D6 polymorphisms.
- Clinician Education: Effective utilization of the tool would necessitate additional training for healthcare providers in interpreting genetic data and using the software.
- Ethical Considerations: The use of genetic information in prescribing raises ethical questions about data privacy and potential discrimination.
Conclusion
This study marks a major progress toward more exact and customized pain treatment techniques. Although further validation and improvement are required, patient care may be much improved. As pharmacogenomics develops, instruments like the one created by Saab and Nakad could become essential for safe and efficient opioid prescription policies.
Briefly
Codeine is an opioid analgesic used to treat mild to moderate pain and suppress coughing. Bonding to mu-opioid receptors, it functions on the central nervous system. Codeine is metabolised as a prodrug to morphine, mostly in charge of its pain-relieving properties. Because of genetic variations in metabolism, each person finds different effectiveness and safety profile. Using codeine calls for careful weighing of possible adverse effects, interactions, and dependency risk. Recent studies concentrate on creating safer substitutes and best dosage techniques.
enofmedicines.com
ATTENTION: It is crucial never to take medication without a qualified doctor’s supervision. Always read the Patient Information Leaflet (PIL) with each prescribed medicine. Pharmaceutical companies accurately describe each product’s details, which may be regularly updated, though variations may exist depending on the drug’s composition. This article analyses the active ingredient/s rather than specific brand names containing this generic medicine. Study the instruction leaflet for each preparation you use. Close cooperation with your doctor and pharmacist is vital. Self-administering medication carries serious health risks and must be strictly avoided.
Bibliography
- Hockenhull, Joanna, et al. “The association between the availability of over the counter codeine and the prevalence of non-medical use.” European Journal of Clinical Pharmacology, vol. 78, 2022, pp. 1011-1018. link.springer.com
- Saab, Yolande, and Zahi Nakad. “A software tool to adjust codeine dose based on CYP2D6 gene-pair polymorphisms and drug-drug interactions.” The Pharmacogenomics Journal, vol. 23, 2023, pp. 217-224. www.nature.com
- Sodeifian, Gholamhossein, et al. “Studies on solubility measurement of codeine phosphate (pain reliever drug) in supercritical carbon dioxide and modeling.” Scientific Reports, vol. 13, 2023, Article number: 21020. www.nature.com
- Zarin, Mona Kamelan Zargar, et al. “Synthesis and Modification of Morphine and Codeine, Leading to Diverse Libraries with Improved Pain Relief Properties.” Pharmaceutics, vol. 15, no. 6, 2023, p. 1779. www.mdpi.com
FAQ
What are the main side effects of codeine?
Common side effects of codeine include constipation, nausea, drowsiness, and dizziness. Some users may experience itching or dry mouth. More serious side effects can include respiratory depression, especially in individuals who are ultra-rapid metabolizers. It's crucial to consult a healthcare provider about any persistent or severe side effects.
Is codeine the most powerful painkiller?
No, codeine is not the most powerful painkiller. It's considered a mild to moderately strong opioid, less potent than drugs like morphine or oxycodone. Codeine's effectiveness varies among individuals due to genetic differences in metabolism. For severe pain, stronger opioids or alternative treatments may be prescribed. Always consult a doctor for appropriate pain management.
Is codeine weak or strong?
Codeine is generally classified as a weak to moderately strong opioid. Its potency falls between over-the-counter pain relievers and stronger prescription opioids. The drug's strength can vary based on individual metabolism, particularly CYP2D6 enzyme activity. For some, codeine may provide effective pain relief, while others might require alternative medications. Medical guidance is essential for proper pain management.
Is codeine good for sleep?
While codeine can cause drowsiness, it's not recommended as a sleep aid. Its sedative effects are a side effect rather than an intended use. Using codeine for sleep can lead to dependency and interfere with natural sleep patterns. Additionally, it may mask underlying sleep issues. For sleep problems, consult a healthcare provider for appropriate treatments that address the root cause.
How long does codeine stay in your system?
Codeine typically remains detectable in the body for 1-4 days, depending on factors like dosage, frequency of use, and individual metabolism. It can be detected in urine for up to 48 hours, in blood for about 24 hours, and in saliva for 1-4 days. Hair tests may show codeine use for several months. Always follow prescribed dosing and consult a doctor with concerns.
Can you take codeine with other medications?
Codeine can interact with various medications, potentially altering its effectiveness or increasing side effects. It's particularly important to avoid combining codeine with other central nervous system depressants, including alcohol and certain antidepressants. Always inform your healthcare provider about all medications you're taking, including over-the-counter drugs and supplements, to prevent harmful interactions.
How does codeine compare to other pain relievers?
Codeine is milder than strong opioids like morphine but more potent than over-the-counter pain relievers such as ibuprofen. Its effectiveness can vary significantly between individuals due to genetic factors affecting metabolism. For some, codeine provides adequate pain relief, while others may require alternatives. The choice of pain reliever should be made in consultation with a healthcare professional based on specific needs and medical history.