Generic Name: Metoprolol
Brand Names: Various around the world
Drug Class: Beta-blocker
Metoprolol Side Effects, Uses, Dosage, and More
What is Metoprolol?
Metoprolol is a medication that belongs to a class of drugs called beta-blockers. It is primarily used to treat high blood pressure (hypertension), angina (chest pain), heart failure, and to prevent heart attacks. This medication works by blocking the effects of epinephrine, also known as adrenaline, on the heart and blood vessels. By doing so, it helps to lower heart rate, blood pressure, and cardiac workload.
Metoprolol is available in various formulations, including immediate-release and extended-release tablets, as well as injectable forms. Many pharmaceutical companies worldwide manufacture and distribute metoprolol under different brand names. However, the active ingredient remains the same regardless of the brand.
Mechanism of action: Metoprolol selectively blocks beta-1 adrenergic receptors in the heart, reducing its rate and contractility. This action leads to decreased cardiac output and lower blood pressure.
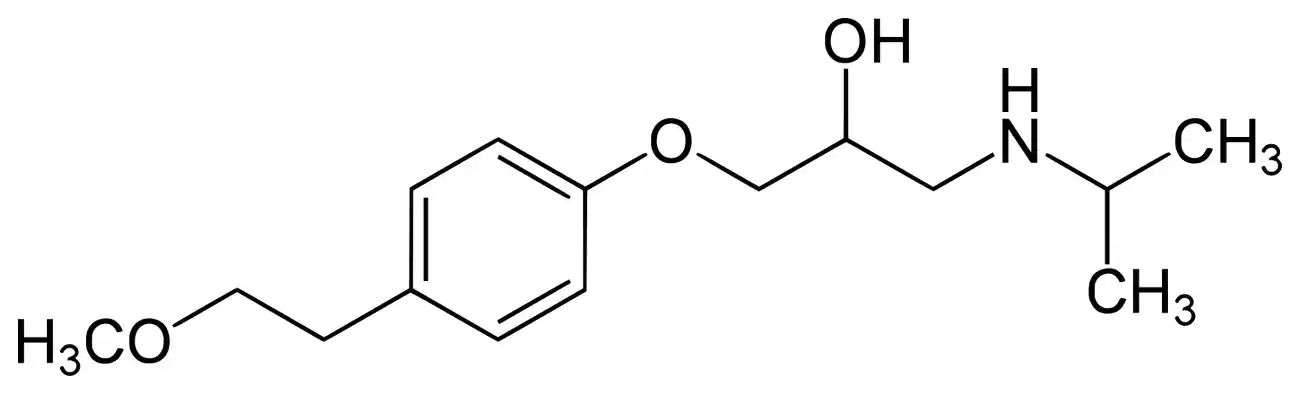
Chemical structure: Metoprolol is a synthetic compound with the chemical formula C15H25NO3.
Therapeutic category: Antihypertensive, antianginal, and antiarrhythmic agent.
Anatomical/therapeutic/chemical (ATC) classification
ATC Code: C07AB02 Title: Metoprolol Classification: Cardiovascular system, Beta blocking agents, Beta blocking agents, selective
History of Medicine
Researchers at the Swedish pharmaceutical firm Hässle AB, which subsequently merged with AstraZeneca, first created metoprolol in the 1960s. It was first granted a patent in 1968, and in 1978 the US government authorized its usage for medicinal purposes. The emergence of metoprolol signified a noteworthy progression in the management of cardiovascular ailments, providing a more tailored beta-blocker in contrast to previous drugs within this category.
In this article, we will analyze several recent studies on metoprolol, including a systematic review of its clinical pharmacokinetics by Zamir et al., published in Clinical Pharmacokinetics, and a meta-analysis comparing intravenous diltiazem and metoprolol for atrial fibrillation by Lan et al., published in The American Journal of Emergency Medicine. These studies provide valuable insights into the efficacy and clinical applications of metoprolol in various cardiovascular conditions.
Indications of Metoprolol
Metoprolol, a selective beta-1 blocker, is prescribed for various cardiovascular conditions. Its primary indications include:
- Hypertension management
- Angina pectoris treatment
- Heart failure therapy
- Post-myocardial infarction care
- Arrhythmia control, particularly supraventricular tachycardia
In a meta-analysis by Lan et al. published in The American Journal of Emergency Medicine, researchers found that intravenous metoprolol showed efficacy in managing atrial fibrillation with rapid ventricular rate. The study noted, “Compared with intravenous metoprolol, intravenous diltiazem was found higher efficacy, shorter average onset time, lower ventricular rate, less impact on systolic blood pressure.” This highlights the drug’s utility in specific cardiac rhythm disorders.
Contraindications and Precautions
Metoprolol should not be used in patients with:
- Severe bradycardia
- Heart block greater than first degree
- Cardiogenic shock
- Severe peripheral arterial disease
- Pheochromocytoma (without alpha-blocker coverage)
- Hypersensitivity to metoprolol or other beta-blockers
Caution is advised in patients with bronchospastic diseases, diabetes, and thyroid disorders.
Special Warnings for the Elderly, Children and Pregnant Women
Elderly patients may be more sensitive to metoprolol’s effects and require lower initial doses. Children’s safety and efficacy data are limited, necessitating careful consideration before use. Pregnant women should only use metoprolol when clearly needed, as it may pose risks to the fetus, particularly in the third trimester.
Dosage and Administration
Dosage varies based on the condition being treated and individual patient factors. Generally, treatment begins with lower doses, gradually increasing as needed. For hypertension, a typical starting dose might be 25-100 mg daily, while heart failure treatment often starts at 12.5-25 mg twice daily.
What Should I Do If I Miss a Dose?
If a dose is missed, it should be taken as soon as remembered. However, if it’s close to the next scheduled dose, skip the missed dose and resume the regular schedule. Double doses should be avoided.
Uses of Metoprolol
Beyond its primary cardiovascular indications, metoprolol has shown utility in:
- Migraine prophylaxis
- Management of certain anxiety disorders
- Treatment of hyperthyroidism symptoms
Kleinbongard et al., in their study published in Basic Research in Cardiology, explored metoprolol’s potential in reducing infarct size. They noted, “Whereas prior experiments in juvenile pigs had reported infarct size reduction by intravenous metoprolol early during myocardial ischaemia, two major clinical trials in patients with reperfused acute myocardial infarction were equivocal.” This highlights the ongoing research into expanding metoprolol’s therapeutic applications.
Overdose
Metoprolol overdose can lead to severe bradycardia, hypotension, bronchospasm, and in extreme cases, cardiogenic shock. Treatment typically involves supportive care, gastric lavage if recently ingested, and specific interventions like atropine for bradycardia or glucagon for refractory hypotension.
Interactions
Drug-Drug Interactions
Metoprolol interacts with various medications, potentially altering its efficacy or increasing side effect risks. Key interactions include:
- Calcium channel blockers: May enhance negative inotropic and chronotropic effects
- Antiarrhythmics: Can potentiate cardiac effects
- CYP2D6 inhibitors: May increase metoprolol blood levels
- Insulin and oral antidiabetics: May mask hypoglycemia symptoms
Zamir et al., in their systematic review published in Clinical Pharmacokinetics, emphasized the importance of understanding these interactions: “Twenty different studies have reported significant changes in CL, Cmax, and AUC of metoprolol when it is co-administered with other drugs.”
Drug-Food Interactions
While metoprolol can generally be taken with or without food, certain dietary considerations exist:
- High-fat meals may increase drug absorption
- Grapefruit juice can potentially increase metoprolol blood levels
- Alcohol consumption should be limited due to potential hypotensive effects
It’s crucial for patients to discuss all medications, supplements, and dietary habits with their healthcare provider to ensure safe and effective metoprolol use.
Metoprolol Side Effects
While metoprolol is generally well-tolerated, it can produce various adverse reactions. Understanding these potential side effects is crucial for patients and healthcare providers alike. Common side effects often relate to the drug’s mechanism of action and may include:
- Fatigue or weakness
- Dizziness
- Bradycardia (slow heart rate)
- Cold hands and feet
- Gastrointestinal disturbances
In their systematic review, Zamir et al. highlight the importance of monitoring these effects, noting that “The summarized pharmacokinetic data presented in this review can assist in developing and evaluating pharmacokinetic models of metoprolol. Moreover, this data can provide practitioners with an insight into dosage adjustments among the diseased populations and can assist in preventing potential adverse drug reactions“ (Clinical Pharmacokinetics).
More specific cardiovascular effects may occur, particularly in patients with pre-existing heart conditions. Lan et al.’s meta-analysis comparing metoprolol to diltiazem for atrial fibrillation observed that “Intravenous diltiazem has higher efficacy, shorter average onset time, lower ventricular rate, less impact on blood pressure, and with no increase in adverse events compared to intravenous metoprolol” (The American Journal of Emergency Medicine). This suggests that while metoprolol is effective, it may have more pronounced effects on blood pressure and heart rate compared to some alternatives.
Respiratory symptoms, such as shortness of breath or wheezing, can occur, especially in patients with a history of asthma or chronic obstructive pulmonary disease (COPD). These effects stem from beta-blockade in the lungs, although metoprolol’s selectivity for beta-1 receptors somewhat mitigates this risk compared to non-selective beta-blockers.
Rare but Possible Metoprolol Side Effects
While less common, some patients may experience more severe adverse reactions:
- Severe allergic reactions (anaphylaxis)
- Depression or mood changes
- Visual disturbances
- Hepatotoxicity
- Severe skin reactions
Kleinbongard et al.’s study in Basic Research in Cardiology, while focusing on metoprolol’s cardioprotective effects, also touched on potential adverse outcomes. They observed that “With an additional dose of 1 mg kg−1 metoprolol after 30-min ischaemia in 4 additional pigs, infarct size was also not reduced (54 ± 9% vs. 46 ± 8% in 3 contemporary placebo, n.s.), and area of no-reflow tended to be increased (59 ± 20% vs. 29 ± 12%, n.s.)”. This highlights the complex nature of metoprolol’s effects and the potential for unexpected outcomes in certain situations.
In rare cases, metoprolol may paradoxically exacerbate the conditions it’s meant to treat, such as worsening heart failure or causing severe bradycardia. These effects underscore the need for careful patient monitoring, especially when initiating therapy or adjusting dosages.
How to Manage Metoprolol Side Effects
Managing side effects often involves a combination of dosage adjustments, lifestyle modifications, and in some cases, additional medications. Here are some strategies:
- Gradual Dose Titration: Starting with a low dose and gradually increasing it can help minimize side effects. As Zamir et al. note, “The oral studies depict a dose-dependent increase in maximum plasma concentration (Cmax), time to reach maximum plasma concentration (Tmax), and area under the concentration–time curve (AUC)” (Clinical Pharmacokinetics). This suggests that careful dose adjustment can significantly impact both efficacy and side effect profile.
- Timing of Administration: Taking metoprolol with food or at bedtime may help alleviate certain side effects like dizziness or gastrointestinal disturbances.
- Regular Monitoring: Frequent check-ups, especially in the initial stages of treatment, allow for timely detection and management of adverse effects. This is particularly important for elderly patients or those with comorbidities.
- Lifestyle Modifications: Encouraging patients to maintain adequate hydration, avoid sudden position changes, and engage in regular light exercise can help mitigate side effects like dizziness and fatigue.
- Patient Education: Informing patients about potential side effects and when to seek medical attention is crucial. For instance, patients should be aware that abruptly stopping metoprolol can lead to rebound hypertension or worsening angina.
- Adjunctive Therapies: In some cases, additional medications may be prescribed to counteract specific side effects. For example, laxatives might be recommended for constipation.
- Consider Alternative Formulations: Extended-release formulations of metoprolol may provide more stable blood levels and potentially fewer side effects compared to immediate-release versions.
It’s important to note that while managing side effects is crucial, the benefits of metoprolol often outweigh the risks for many patients. As Yang et al. point out in their study on metoprolol transformation, “Metoprolol is recommended for therapeutic use in multiple cardiovascular conditions, thyroid crisis, and circumscribed choroidal hemangioma” (Journal of Hazardous Materials). This underscores the drug’s importance in treating various conditions, despite potential side effects.
Patients should always consult their healthcare provider before making any changes to their metoprolol regimen. Open communication about experienced side effects is essential for optimal management and ensuring the best possible outcomes from metoprolol therapy.
Additional Important Information of Metoprolol
Metoprolol, a widely prescribed beta-blocker, has been the subject of extensive research and clinical use. Its efficacy in treating various cardiovascular conditions is well-established, yet ongoing studies continue to refine our understanding of its mechanisms, applications, and potential limitations.
Resistance Development
Although pharmacological resistance to metoprolol is not very prevalent, many factors may affect its efficacy over time. Variability in medication response may result from genetic polymorphisms especially impacting the CYP2D6 enzyme in charge of metoprolol metabolism. Published in Clinical Pharmacokinetics, Zamir et al.’s systematic study “CYP2D6 polymorphism and its impact on the clinical response to metoprolol: a systematic review and meta-analysis” observed notable differences in metoprolol’s pharmacokinetics depending on CYP2D6 genotypes.
Long-term usage also results in physiological changes. Some patients may find their drug’s efficacy gradually declining, in which case dosage changes or combination treatments are necessary. Not exclusive to metoprolol, this phenomena—often known as “beta-blocker tolerance—is seen across the beta-blocker class.
Preclinical and Clinical Studies
Preclinical research has shed important light on possible novel uses and the modes of action of metoprolol. Particularly helpful in clarifying the effects of the medication on heart tissue under many circumstances are animal models. In their Basic Research in Cardiology paper, Kleinbongard et al. performed tests on Göttingen minipigs to evaluate how metoprolol affected infarct size and no-reflow phenomena. Their results—which revealed “no robust reduction of infarct size and no-reflow by metoprolol pretreatment”—showcase the difficulty of converting preclinical data to clinical practice.
Clinical studies have helped us to better grasp the safety and effectiveness profile of metoprolol. A historic investigation, the METOCARD-CNIC experiment looked at early intravenous metoprolol’s cardioprotective benefits on ST-segment elevation myocardial infarction patients. Nevertheless, other trials like as the EARLY-BAMI trial yielded contradicting findings, which emphasizes the importance of ongoing research to maximize metoprolol usage in acute cardiac environments.
Published in The American Journal of Emergency Medicine, Lan et al.’s meta-analysis compared intravenous metoprolol with diltiazem for atrial fibrillation with fast ventricular rate. Their results imply that while both drugs have benefits, diltiazem could have some in terms of start time and influence on ventricular rate. Clinics may benefit much from this comparative approach in choosing suitable therapies for certain patient groups.
Post-authorization Studies and Pharmacovigilance
Identification of unusual side effects and long-term safety issues has depend critically on post-marketing monitoring of metoprolol. Although they may not have been evident in first clinical trials, pharmacovigilance systems have helped to identify and control unusual side events like severe cutaneous responses or hepatotoxicity.
Large-scale observational studies have given real-world information on the safety and efficacy of metoprolol among several patient categories. Particularly helpful in evaluating the drug’s effectiveness among older patients, those with numerous comorbidities, and in different ethnic groups—populations often underrepresented in controlled clinical trials—have been these investigations.
Big data and electronic health records’ arrival has made more thorough studies of metoprolol’s long-term consequences easier. These trials have helped us to better grasp how the medication affects quality of life, cardiovascular results, and mortality in people with chronic diseases like hypertension and heart failure.
One exciting field of study in maximizing metoprolol treatment is pharmacogenomic research. Research on genetic differences in beta-adrenergic receptors and metabolizing enzymes seeks to customize treatment plans, therefore improving effectiveness and maybe reducing side effects.
More recently, research on fresh uses for metoprolol has looked at Published in the Journal of Hazardous Materials, Yang et al. investigated the metoprolol transformation in UV/PDS systems, therefore providing information on the environmental destiny of this frequently used drug. This study emphasizes the need of examining the wider ecological effect of medicinal drugs.
The use of metoprolol in contemporary therapy changes along with our knowledge of cardiovascular pathophysiology. Dosing techniques are still being refined by constant study, which also looks at possible synergies with other drugs and their use in treating newly arising cardiovascular problems. The abundance of information gathered over decades of clinical usage and study reveals metoprolol as a well-known yet continually developing tool in the treatment of cardiovascular diseases.
Pharmacokinetic Characteristics of Metoprolol
Complicated pharmacokinetic characteristics of metoprolol greatly affect both its therapeutic effectiveness and its side effects. Extensive research on the absorption, distribution, metabolism, and excretion characteristics of the medication has produced significant new information for use in clinics.
Usually reaching peak plasma concentrations one to two hours after delivery, oral absorption of metoprolol is quick and almost complete. Still, significant first-pass metabolism alters the bioavailability. “The oral studies depict a dose-dependent increase in maximum plasma concentration (Cmax), time to reach maximum plasma concentration (Tmax), and area under the concentration–time curve (AUC),” said Zamir et al., in their methodical review written for Clinical Pharmacokinetics. This point emphasizes in practical practice the need of dosage titration.
With a volume of distribution between 3.2 and 5.6 L/kg, metoprolol is distributed extensively throughout bodily tissues. The medicine passes the blood-brain barrier and placenta, hence pregnant patients should give much thought. Protein binding is quite modest at around 12%, which helps to explain its wide dispersion in tissues.
Metoprolol mostly metabolizes in the liver via the cytochrome P450 2D6 (CYP2D6) enzyme. There is notable genetic variation in this system, which results in somewhat high inter-individual variability in medication response. According to Zamir et al., “CYP2D6 polymorphism and its impact on the clinical response to metoprolol: a systematic review and meta-analysis” showed significant differences in metoprolol’s pharmacokinetics depending on CYP2D6 genotypes. Poor, moderate, extensive, or ultra-rapid metabolizer phenotypes—each with unique consequences for dose and efficacy—can arise from this genetic heterogeneity.
With about 95% of an oral dosage removed in urine, metoprolol and its metabolites are excuted mostly via the kidneys. In normal metabolizers, the half-life of elimination usually falls between three and seven hours; in individuals with hepatic or renal disease, this range may be much extended.
Current Research Directions and Future Perspectives
From molecular pharmacology to therapeutic uses and environmental effects, current studies on metoprolol are diverse. The possible neuroprotective properties of the medication provide one growing topic of research. Particularly in those with cardiovascular problems, studies are looking at metoprolol’s ability to lower the risk of cognitive decline and dementia.
With an eye toward customizing metoprolol treatment depending on genetic profiles, personalized medicine techniques are becoming popular. Including pharmacogenomic data into clinical decision-making instruments has great potential to maximize therapy results and reduce side effects.
Research focus is also being shaped by environmental issues. Yang et al. examined the “Transformation of metoprolol in UV/PDS process: Role and mechanisms of degradation and polymerization” in their work written for the Journal of Hazardous Materials. This study emphasizes the rising need in knowing the environmental destiny of drugs and creating plans for their safe breakdown in water treatment systems.
Future directions call for the development of new drug delivery technologies to improve patient compliance and pharmacokinetic profile of metoprolol. Active research topics include transdermal delivery techniques and extended-release formulations.
Effectiveness
Extensive clinical experience and studies confirm that metoprolol is very helpful in controlling different cardiovascular diseases. Its main modes of action—reduction of heart rate, cardiac contraction, and blood pressure—help to explain why it treats heart failure, angina, and hypertension well.
In acute circumstances, including the treatment of atrial fibrillation with fast ventricular response, metoprolol has demonstrated notable potency. In their meta-analysis written for The American Journal of Emergency Medicine, Lan et al. compared intravenous metoprolol to diltiazem and found that, while both medications were beneficial, metoprolol exhibited particular benefits in several clinical situations.
Large-scale clinical studies, particularly in patients with heart failure and post-myocardial infarction, have shown long-term efficacy of metoprolol in lowering cardiovascular morbidity and death. Individual pharmacogenomic profiles, patient adherence, and dosage schedule may all affect the efficacy of the medication, however.
Comparative Efficacy, Systematic Reviews and Meta-analyses
Comparative studies have shed important light on the relative effectiveness of metoprolol to other cardiovascular drugs. Lan et al.’s meta-analysis, in the framework of atrial fibrillation care, showed ” Compared with intravenous metoprolol, intravenous diltiazem was found higher efficacy, shorter average onset time, lower ventricular rate, less impact on systolic blood pressure.” For urgent cardiovascular treatment, this result provides significant clinical direction.
Data from several clinical studies have been integrated in systematic reviews to provide a whole picture of metoprolol’s effectiveness in many conditions. These studies repeatedly show how well the medication controls secondary prevention after a myocardial infarction and manages hypertension.
Meta-analyses have also looked at metoprolol’s place in certain therapeutic settings. Studies of its usage in perioperative cardiac risk reduction, for example, have shown conflicting findings that emphasize the necessity of cautious patient selection and timing of treatment.
In a pig model of myocardial infarction, Kleinbongard et al., in their Basic Research in Cardiology paper, performed a critical investigation of metoprolol’s cardioprotective actions. Their discovery that “infarct size reduction by metoprolol in pigs is not robust, and this result reflects the equivocal clinical trials” emphasizes the difficulty of converting preclinical results to clinical practice and the need of thorough, well-planned investigations.
The changing field of cardiovascular therapy constantly forces review of metoprolol’s role in treatment plans. Constant comparison studies including more modern medicines, including new beta-blockers and other antihypertensive classes, help us to better grasp the relative effectiveness and best usage of metoprolol in modern clinical practice.
Analysis of the Research Study “Clinical Pharmacokinetics of Metoprolol: A Systematic Review”
This comprehensive systematic review, conducted by Ammara Zamir, Iltaf Hussain, Anees ur Rehman, Waseem Ashraf, Imran Imran, Hamid Saeed, Abdul Majeed, Faleh Alqahtani, and Muhammad Fawad Rasool, was published in Clinical Pharmacokinetics in 2022. The study aimed to consolidate and analyze the existing literature on metoprolol’s pharmacokinetics, providing a valuable resource for clinicians and researchers alike.
Methodology
The researchers employed a rigorous methodology, searching Google Scholar and PubMed databases for articles related to metoprolol’s clinical pharmacokinetics. Their inclusion criteria were stringent, focusing on studies that reported:
- Plasma concentration-time profiles
- Various routes of administration (intravenous and oral)
- At least one pharmacokinetic parameter
This approach ensured a comprehensive yet focused analysis of the available data.
Key Findings
The review yielded several significant findings:
- Dosage Forms: The study analyzed data from both immediate-release and controlled-release formulations, providing a comprehensive view of metoprolol’s pharmacokinetics across different dosage forms.
- Dose-Dependent Kinetics: A notable observation was the “dose-dependent increase in maximum plasma concentration (Cmax), time to reach maximum plasma concentration (Tmax), and area under the concentration–time curve (AUC)” for oral administration. This finding has important implications for dosing strategies in clinical practice.
- Enantiomer Differences: The review highlighted differences between R- and S-enantiomers of metoprolol, with S-metoprolol showing higher values of Cmax, Tmax, and AUC. This observation underscores the complexity of metoprolol’s pharmacokinetics and potential implications for its pharmacodynamic effects.
- Disease State Impacts: The researchers found significant differences in metoprolol’s pharmacokinetics in various disease states. For instance, patients with renal impairment showed increased clearance compared to healthy subjects, while those with hepatic cirrhosis exhibited decreased clearance.
- Drug Interactions: The review identified twenty different studies reporting significant changes in metoprolol’s pharmacokinetics when co-administered with other drugs. This finding emphasizes the importance of considering potential drug interactions in clinical practice.
Critical Analysis
The thorough approach and exact technique of this systematic study define its strength. The authors have created a streamlined resource with insights on metoprolol’s behavior across many patient demographics and clinical situations by aggregating data from several research.
The report also emphasizes, nevertheless, gaps in the present body of research. For certain patient groups, like juvenile patients or those with particular comorbidities, the writers point out little information. This insight suggests topics for further study.
Especially helpful are the results of the review on illness state effects and medication interactions. These revelations might help doctors predict possible medication interactions and alter doses for individuals with renal or hepatic impairment.
Implications for Clinical Practice
The study’s findings have several important implications for the clinical use of metoprolol:
- The dose-dependent pharmacokinetics suggest that careful dose titration may be necessary to achieve optimal therapeutic effects while minimizing side effects.
- The observed differences between R- and S-enantiomers raise questions about the potential benefits of enantiomer-specific formulations in the future.
- The data on disease state impacts underscores the need for dose adjustments in patients with renal or hepatic impairment.
- The extensive information on drug interactions provides valuable guidance for avoiding potential adverse effects when prescribing metoprolol alongside other medications.
In conclusion, this systematic review by Zamir et al. represents a significant contribution to our understanding of metoprolol’s clinical pharmacokinetics. By synthesizing data from numerous studies, it provides a comprehensive resource that can inform both clinical decision-making and future research directions in cardiovascular pharmacology.
Briefly
Metoprolol, a widely prescribed beta-blocker, plays a crucial role in managing various cardiovascular conditions. This drug reduces blood pressure and heart rate by thereby inhibiting the effects of adrenaline on the heart. Its adaptability reaches to treating heart failure, angina, hypertension, and heart attacks prevention. Although metoprolol is typically well-tolerated, its side effects and interactions call for close physician monitoring and tailored dose schedules to maximize therapeutic results and reduce unpleasant events.
enofmedicines.com
ATTENTION: It is crucial never to take medication without a qualified doctor’s supervision. Always read the Patient Information Leaflet (PIL) with each prescribed medicine. Pharmaceutical companies accurately describe each product’s details, which may be regularly updated, though variations may exist depending on the drug’s composition. This article analyses the active ingredient/s rather than specific brand names containing this generic medicine. Study the instruction leaflet for each preparation you use. Close cooperation with your doctor and pharmacist is vital. Self-administering medication carries serious health risks and must be strictly avoided.
Bibliography
- Kleinbongard, P., et al. “No robust reduction of infarct size and no-reflow by metoprolol pretreatment in adult Göttingen minipigs.” Basic Research in Cardiology, vol. 118, no. 23, 2023, link.springer.com
- Lan, Q., et al. “Intravenous diltiazem versus metoprolol for atrial fibrillation with rapid ventricular rate: A meta-analysis.” The American Journal of Emergency Medicine, vol. 51, 2022, pp. 248-256, sciencedirect.com
- Yang, S.Q., et al. “Transformation of metoprolol in UV/PDS process: Role and mechanisms of degradation and polymerization.” Journal of Hazardous Materials, vol. 472, 2024, Article 134498, sciencedirect.com
- Zamir, A., et al. “Clinical Pharmacokinetics of Metoprolol: A Systematic Review.” Clinical Pharmacokinetics, vol. 61, 2022, pp. 1095-1114, link.springer.com
FAQ
What is the difference between metoprolol succinate and tartrate?
Metoprolol succinate is an extended-release formulation, typically taken once daily, while metoprolol tartrate is immediate-release and usually taken twice daily. Succinate provides more stable blood levels over 24 hours, potentially improving efficacy and reducing side effects. However, the choice between them depends on individual patient needs and should be determined by a healthcare provider.
What are the common side effects of metoprolol?
Common metoprolol side effects include fatigue, dizziness, slow heart rate, and cold hands and feet. Some patients may experience gastrointestinal issues or sleep disturbances. It's crucial to report any persistent or severe side effects to your doctor. Remember, not everyone experiences these effects, and many find the benefits outweigh the risks.
How does metoprolol work in the body?
Metoprolol is a beta-blocker that works by blocking the effects of adrenaline on the heart and blood vessels. It slows heart rate, reduces cardiac workload, and lowers blood pressure. This action helps manage conditions like hypertension, angina, and heart failure. Always consult your doctor for personalized information about how this medication affects your specific condition.
What precautions should elderly patients take when using metoprolol?
Elderly patients may be more sensitive to metoprolol's effects, particularly dizziness and low blood pressure. They should start with lower doses and be monitored closely for side effects. Regular check-ups are essential to adjust dosage if needed. It's crucial for elderly patients to discuss all medications and health conditions with their doctor before starting metoprolol.
Can metoprolol interact with other medications?
Yes, metoprolol can interact with several medications, including other heart medications, certain antidepressants, and drugs that affect liver enzymes. These interactions can alter metoprolol's effectiveness or increase side effects. It's vital to inform your healthcare provider about all medications, supplements, and herbal products you're taking. Always seek medical advice before starting or stopping any medication.
What is the typical dosage for metoprolol 25 mg?
The typical starting dose of metoprolol 25 mg varies depending on the condition being treated and individual patient factors. For hypertension, it's often 25-100 mg daily, while for heart failure, it might start at 12.5-25 mg twice daily. Dosage adjustments are common and should only be made under medical supervision. Always follow your doctor's prescribed dosage instructions.
How should metoprolol be taken for optimal effectiveness?
For optimal effectiveness, take metoprolol exactly as prescribed by your doctor. Succinate formulations are usually taken once daily, while tartrate is often taken twice daily. It's generally advised to take metoprolol at the same time(s) each day, with or without food. Never stop taking metoprolol abruptly without medical guidance. Regular follow-ups with your healthcare provider ensure the medication's effectiveness.


